You find your dog with an empty tube of horse wormer paste on the floor. Teeth marks puncture the plastic. Flavored gel is smeared on their muzzle. Your heart pounds. What do you do next?
This moment of crisis is not the time to search for information. This article provides a step-by-step first aid guide for suspected ivermectin or macrocyclic lactone exposure. Read it now, before you need it, so the information is fresh when every minute counts.
- ASPCA Animal Poison Control Center: 888-426-4435
- Pet Poison Helpline: 855-764-7661
- Your Emergency Vet: [Add your local 24-hour clinic]
- Your Regular Vet: [Add your veterinarian's number]
A consultation fee applies to poison control calls but is worth every cent in an emergency.
Step 1: Assess the Situation (30 Seconds)
Take a breath. Panic helps no one. You need to think clearly for your dog's sake.
Look at your dog. Are they acting normal? Are they already showing symptoms like wobbling, drooling, or trembling? This information matters for the next steps.
Identify what they got into. Grab the container, package, or remaining product. You will need this information for veterinary staff and poison control. Even partial labels help.
Estimate how much is missing. Compare the original amount (often on the label) to what remains. This helps calculate the exposure dose. Even a rough estimate is better than no estimate.
Step 2: Call for Professional Guidance (Immediately)
Call your veterinarian or emergency clinic first if they are readily available. They can provide immediate guidance and prepare for your arrival.
If you cannot reach a veterinarian immediately, call ASPCA Animal Poison Control (888-426-4435) or Pet Poison Helpline (855-764-7661). These services are staffed by veterinary toxicologists who can advise on immediate actions and whether emergency care is needed.
Have the following information ready:
- Your dog's weight
- Your dog's breed and MDR1 status if known
- The product name and active ingredient
- The concentration of the product if available
- Your estimate of how much was ingested
- The time of ingestion if known
- Any symptoms your dog is showing
Information to Gather Before Calling
Dog information: Weight, breed, age, MDR1 status
Product information: Brand name, active ingredient, concentration (mg/mL or percentage)
Exposure information: Amount missing, time of ingestion, route (oral, topical, injection)
Current status: Symptoms present, normal behavior, or signs of concern
Step 3: Decontamination Decisions
Decontamination means removing the toxin before it is fully absorbed. For oral ingestions, this primarily means inducing vomiting. But inducing vomiting is not always safe and should only be done with professional guidance.
When Inducing Vomiting May Be Appropriate
- Ingestion occurred within the past 1 to 2 hours
- Dog is fully alert and responsive
- Dog is not showing neurological symptoms
- Dog has a normal gag reflex
- A veterinarian or poison control has recommended it
When NOT to Induce Vomiting
- Dog is already showing neurological symptoms (wobbling, trembling, drooling excessively, dilated pupils)
- Dog is lethargic, sedated, or unconscious
- Dog is having difficulty breathing
- Ingestion was more than 2 to 3 hours ago (drug already absorbed)
- You have not spoken to a veterinarian or poison control
How to Induce Vomiting (If Recommended by a Professional)
If and only if a veterinarian or poison control has specifically recommended inducing vomiting, hydrogen peroxide is the standard home method.
Use 3% hydrogen peroxide only. The concentration found in most household first aid kits is appropriate. Do not use higher concentrations or hair product peroxide.
The dose is 1 teaspoon (5 mL) per 10 pounds of body weight, with a maximum of 3 tablespoons (45 mL) regardless of dog size. Administer orally using a syringe, turkey baster, or spoon directed toward the back of the mouth.
Walk your dog around after administration. Movement stimulates vomiting. Most dogs vomit within 10 to 15 minutes. If no vomiting occurs after 15 minutes, the dose can be repeated once.
Collect the vomit if possible. It may help veterinary staff assess how much product was expelled.
Step 4: Topical Exposure Response
If your dog was exposed to a topical ivermectin product like pour-on cattle formulations, decontamination means removing the product from their skin and coat.
Bathe your dog thoroughly with liquid dish soap. Dawn or similar degreasing dish soap works well. Lather thoroughly, leave on for several minutes, then rinse completely. Repeat 2 to 3 times if significant product was applied.
Wear gloves during bathing to avoid absorbing the product through your own skin.
Even with thorough bathing, some absorption may have already occurred. Continue to monitor for symptoms and seek veterinary care if any concern develops.
Step 5: Transport to Veterinary Care
Significant exposures require veterinary evaluation even if your dog currently appears normal. Symptoms can take hours to develop, and early intervention improves outcomes.
Bring the product container with you. The veterinary team needs to verify the active ingredient, concentration, and calculate the exposure dose accurately.
Keep your dog calm during transport. Minimize stimulation. If your dog is showing symptoms, handle them gently and support them to prevent injury if they are unsteady.
If your dog vomits during transport, try to prevent them from re-ingesting the vomit. Keep their head positioned to prevent aspiration.
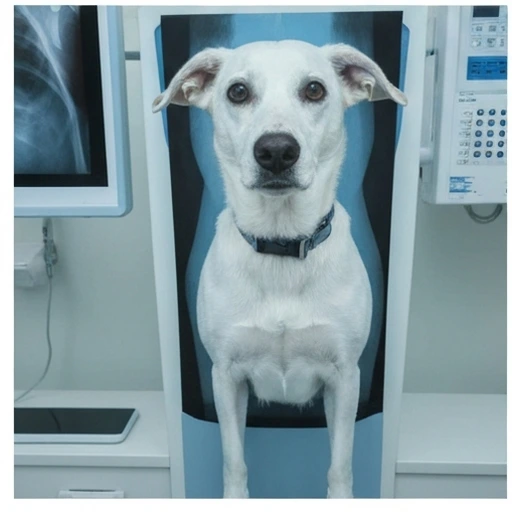
Step 6: What to Expect at the Veterinary Clinic
The veterinary team will assess your dog's neurological status, vital signs, and overall condition. They will calculate the exposure dose based on the product and amount ingested.
If your dog is not yet showing symptoms, they may administer activated charcoal to bind any remaining drug in the gastrointestinal tract and reduce further absorption.
If symptoms are present, treatment focuses on supportive care. This may include IV fluids, medications to control seizures if present, temperature management, and monitoring. In moderate to severe cases, intravenous lipid emulsion therapy may be initiated. For detailed information on veterinary treatment, see our treatment protocol guide.
Be prepared for the possibility of hospitalization. Moderate to severe toxicity cases often require days of intensive care. The veterinary team will discuss prognosis based on the exposure dose, your dog's MDR1 status if known, and their current clinical condition.
Symptom Timeline: What to Watch For
Ivermectin toxicity symptoms typically develop 4 to 12 hours after oral ingestion, sometimes longer. Knowing what to watch for helps you recognize problems early.
Early Signs (Mild Toxicity)
- Subtle unsteadiness, especially when changing direction
- Dilated pupils
- Increased drooling
- Reduced appetite
- Quieter than normal behavior
Progressive Signs (Moderate Toxicity)
- Obvious wobbling, stumbling, or falling
- Tremors or muscle twitching
- Apparent vision problems (bumping into things)
- Disorientation or confusion
- Vomiting
Severe Signs (Emergency)
- Inability to stand
- Seizures
- Unresponsiveness
- Slow or labored breathing
- Hypothermia (cold to touch)
For a complete guide to recognizing toxicity stages, see our article on clinical signs of ivermectin toxicity.
When to Seek Emergency Care
Go to an emergency veterinary clinic immediately if your dog shows:
- Any neurological symptoms after known exposure
- Progressive worsening of symptoms
- Inability to stand or walk
- Seizure activity
- Unresponsiveness or extreme lethargy
- Difficulty breathing
Do not wait for symptoms to worsen. Earlier treatment leads to better outcomes.
The Waiting Period
If your dog ingested a small amount or received veterinary care and was discharged for home monitoring, the next 24 to 48 hours require vigilance.
Check on your dog every 2 to 4 hours. Watch for any of the symptoms listed above. Keep a log of their status including appetite, activity level, walking ability, and pupil size.
Keep your dog in a quiet, safe environment. Remove hazards they might injure themselves on if they become unsteady. Block access to stairs or elevated furniture.
Do not leave your dog alone for extended periods during the monitoring window. If you must leave, arrange for someone to check on them regularly.
If symptoms develop at any point, return to veterinary care immediately. Mild symptoms can progress rapidly to severe toxicity, especially in MDR1-affected dogs.
If You Do Not Know Your Dog's MDR1 Status
Many exposures happen to dogs who have never been tested for MDR1. If your dog is one of the breeds known to carry the mutation, treat any significant exposure as high-risk.
Breeds with documented MDR1 prevalence include Collies, Australian Shepherds, Shetland Sheepdogs, Border Collies, Old English Sheepdogs, English Shepherds, German Shepherds, Longhaired Whippets, Silken Windhounds, and mixed breeds with ancestry from these breeds.
Even if your dog is not from an at-risk breed, large enough exposures can cause toxicity in any dog. High-concentration livestock products deliver doses that overwhelm even normal P-glycoprotein function.
After your dog recovers, get them tested for MDR1. The information will guide medication decisions for the rest of their life and prevent future emergencies. See our breed prevalence guide for more information on testing.
Preparation for Next Time
Once you have navigated an exposure event, take steps to prevent another:
- Secure all macrocyclic lactone products in locked storage
- Dispose of used containers in secure trash
- Test your dog for MDR1 if not already done
- Update your dog's medical records with the exposure event
- Review our home safety guide for comprehensive prevention strategies
Keep hydrogen peroxide in your pet first aid kit, checking expiration dates regularly. Store emergency contact numbers where they are easily accessible to anyone who might care for your dog.
Key Points to Remember
Stay calm. Your dog needs you thinking clearly.
Call for guidance before acting. Poison control or your veterinarian can advise whether decontamination is appropriate.
Never induce vomiting in a dog showing symptoms. Aspiration risk is too high.
Bring the product container to the vet. Identification and dose calculation depend on it.
Early intervention saves lives. Do not wait to see if symptoms develop.
Monitor closely for 48 hours after exposure, even if initial treatment was given. Delayed symptoms can still occur.
Every exposure event is a wake-up call about prevention. Use it to improve your safety protocols.
The outcome of ivermectin exposure depends heavily on how quickly appropriate action is taken. Dogs who receive prompt decontamination and early supportive care have dramatically better outcomes than those where treatment is delayed. Knowledge is time, and time is survival. Be prepared before you need to be.